Does your child have an ng-tube or g-tube so that they can get the calories and nutrients they need? Kids that have a feeding tube can learn to eat and chew! Get the step-by-step how-to instructions for weaning from tube feedings. Affiliate links used below.
Some children need a feeding tube to eat because they aren’t able to eat or manage their food safely. Or, in some cases, their picky eating becomes very severe. If a child absolutely refuses to eat or eats very little, they may also receive a feeding tube to ensure that they’re getting the calories and nutrition they need.
Initially, many children use a nasogastic tube, or ng-tube, that goes up through their nostril, down the back of their throat and into their stomach. Formula, breast milk, and even very thin liquid foods can be put through the ng-tube.
However, this type of tube is temporary and typically isn’t in place for longer than 6 weeks at the most.
If children continue to need tube feedings, then a procedure to insert a gastrostomy tube, or g-tube is done. This places a port right into the stomach. It’s much easier to manage, but is more permanent, although they can be surgically removed.
Why is Weaning From a G-Tube or NG-Tube Important?
As an occupational therapist that specialized in feeding, I’ve treated children that were placed on a tube feedings. I’ve also supported students through the weaning process in Table Food School and Mealtime Works, depending on their age. What I’ve found is that most children are put on tube feedings with no plan to ever take them off.
There is a peace of mind with tube feedings, because your child that has had difficulty eating now has a direct means for being nourished without any worry of their safety or refusal!
But, most parents would like to see their child resume or learn to eat as other children do. It’s a valuable skill that can enrich a child’s life. It’s also much more convenient, as tubes require maintenance and set up.
When Should You Start Weaning?
When you should start weaning from a g-tube will vary from child to child, but I believe for most kids, you can start preparing the way for weaning as soon as the tube is in place, as this will make the transition to chewing foods a smoother path.
Before you can begin working on any aspect of feeding your child orally, you must check with your doctor, usually their GI doctor. Often, you’ll work with a feeding team to ensure your child is able to safely begin swallowing.
Your child may need a “cookie swallow” or a modified barium swallow. It’s a non-invasive test that takes x-ray pictures of your child eating and swallowing.
A speech language pathologist will closely watch these pictures and determine if eating and/or drinking is safe to attempt.
Even if your child isn’t able to begin eating, there are other important techniques you can begin using that will help them get ready to eat once it’s safe.
How to Start Weaning
I strongly recommend working with a feeding team for the weaning process, I know it’s not always possible. Please stay in close communication with your doctor as a minimum.
Below you’ll learn some of the most beneficial strategies to help you make that transition from tube feeding to oral feeding that seems impossible.
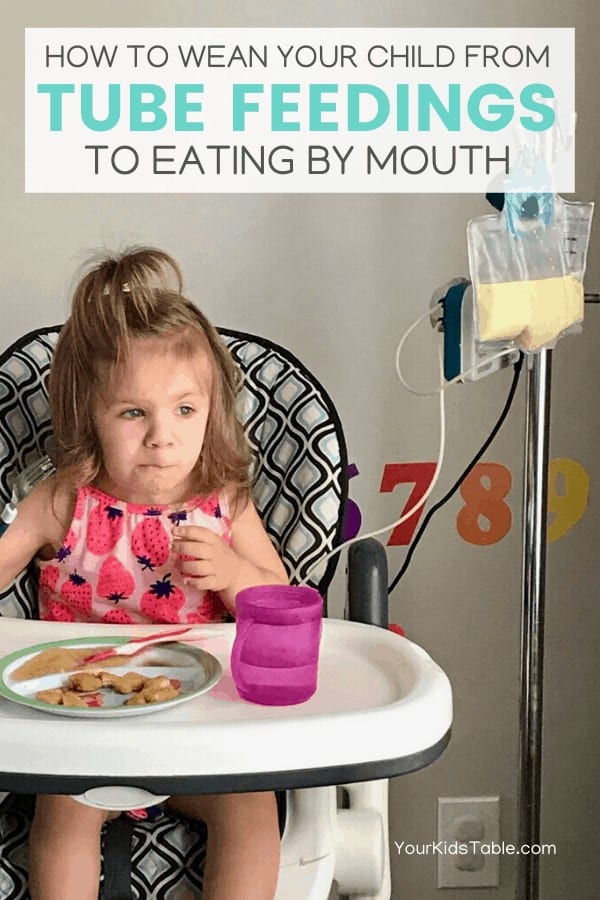
And, I’ve got a powerful real life example to show you, my 2-year old niece Lucy. Although she’s still a baby in this picture…

Lucy got a g-tube at a very early age because of complex medical needs as a result of her Turner’s Syndrome diagnosis. But, my sister Alexis and her husband Aaron began to diligently begin the process of weaning from an early age. Having a sister that’s an OT has some perks 😉
Weaning from tube feedings went slowly at times.
They took breaks when they needed to, or when therapists raised concerns that Lucy might not be swallowing well, and possibly aspirating. That’s one of the biggest concerns with oral feedings, because when a child aspirates, it goes into the lungs not the stomach.
Alexis and Aaron have been kind enough to share some of their personal pictures of some of the strategies I’m going to share with you. It’s been a joy for me to support them through this process. Wait til you hear what Lucy is doing now!
*Note: Even though Lucy is 2, I would use the same strategies for a child at any age beginning to wean from a feeding tube.
Affiliate links used below. See our full disclosure.
Step #1: Oral Play

Many, if not the vast majority of children on feeding tubes, develop strong oral aversions because they aren’t used to having anything in their mouth. We take this for granted because we eat all day long. But, when you don’t have food, bottles, and/or utensils consistently going into your mouth, the whole mouth area becomes sensitive.
Even painful.
Some tube fed kids are also fearful of choking, texture, or taste. They are scared of eating and will refuse to have anything at all near their mouth.
The first step is to get some teethers, a toothbrush, safe toys, or plastic/silicone utensils into their mouth. You’ll likely need to start slow, just touching the tip of the teether to their mouth. Lucy is a using what’s called a z-vibe in this picture. Only use this specific tool if you’re under the guidance of a therapist, as they’re powerful tools that can cause deeper oral aversion if not used correctly.
Practice throughout the day with teethers, a toothbrush, or any other utensil until they can accept these items in their mouth. Encourage them to bite on them and move them around!
This Zoli teether is one of my favorites because it can help address oral aversion and chewing.

You can use this strategy even if your child isn’t able to begin trying food or drink yet.
Read more about how to help kids with oral aversions.
Step #2: Texture Play
Another wrinkle in oral aversion, is sensitivity to texture. If you notice your child gagging at the sight, smell, touch, or even taste of a food or any other texture, they likely are very sensitive to texture. That level of sensitivity makes it very difficult to eat any food.
I address that by encouraging playing and interacting with a wide variety of textures. This can be done away from meals with messy play and sensory bins. The more you child plays in different textures, the more they’ll be tolerant of different textures in their mouth because their brain begins to process textures better with all this exposure.
Set up time to play in different textures daily! Food counts too, again as long as it’s safe if your child puts it in their mouth. The picture below is of Lucy playing with a baby food. She was eating it at this point too.

It’s critical to encourage and allow children with feeding tubes to get as messy as possible. If they’re upset about the mess, clean them up and reassure them. Ultimately, we want them to be able to tolerate being messy.
Step #3: Tasting
As long as you’ve been cleared to start oral feedings, it’s time to start feeding your child small tastes of food. You may need to use your finger or a teether to try those first bites. Spoons sometimes trigger oral aversions.
Focus on tiny little tastes and keep it positive. Smile at your child and make “mmm” sounds. Demonstrate taking a taste yourself.
You will likely work on this stage for a while, working your way up to bigger tastes until they’re eating a few spoonfuls of pureed food. Try baby foods, yogurt, or homemade preferred foods. Just make sure the food is totally smooth. It should have no textures at all.
If your child is having a hard time swallowing, touching their chin to close their mouth can help them swallow the food back instead of spitting it out. See the therapist demonstrating this with Lucy below:

Step #4: Timing
The pivot point to getting your child to understand that they’re hungry is starting to feed them orally when they are tube fed. Most children that have g-tubes or even ng-tubes don’t have a sense of their appetite.
They don’t understand what it feels like to be hungry because food is automatically deposited into their stomach. The brain stops sending signals about hunger. That’s why it’s crucial to match up the timing of the oral and tube feeds.
If your child is on a slow drip feed through the night or day, then you’ll need to talk to your doctor and begin to shift those feeds around. Because the slow feed makes it difficult to connect hunger to eating. Only make tube feeding schedule changes under the guidance of a physician or feeding team that specializes in tube feedings.
As your child begins to eat more orally, you can decrease the amount of food they get from their tube feeding. It’s a bit of a balancing act and does take some time until you’ve found the best balance. The goal is to decrease the amount of nutrition from tube feedings over time until it is eliminated.
Step #5: Eating and Drinking
At this point, volume and variety of foods are usually challenges for a child that is tube fed. To help with volume, eat with your child and demonstrate opening your mouth widely and accepting a bite of food.
You may also want to consider using some high calorie foods so they get the biggest bang for those few spoonfuls of food. Use this list of high calorie foods to get inspired.
As your child accepts purees, you’ll also want to start think about chewing! This is a detailed post that teaches you how to teach your child to chew. Even though it’s geared for younger kids, I’d use the same steps for older kids that haven’t chewed before.
For drinking, you’ll again want to make sure it’s safe to start working on liquids, and if so, which kinds. Milk and formula are thicker than water and therefore easier to manage. Whatever liquid you start with, you’ll want to try putting a little bit on a spoon and seeing how they manage with it. Again, if you’re in feeding therapy, the therapist should try this first.
You’d then keep practicing from a spoon and then experiment with a sippy cup or straw cup (here’s a tutorial on how to teach straw drinking). But, keep in mind that it requires a lot of oral motor skills and sequenced swallowing to do either.
Consistently working on these strategies and being patient with what can be a long process are a very important part of this transition!
Alexis and Aaron focused on these strategies and now, at 2 and 1/2 years old, Lucy is eating just by mouth with no tube feedings for the last 4 months. She’ll need to eat solely by mouth for 6 months before they can begin to discuss plans for removing the g-tube. This time frame does vary though. You can learn more about Lucy’s incredible miracle medical journey here.
Grab a Free Printable
One of the most helpful resources I can give you for this transition is our How to Transition to Table Foods Printable Guide. While this printable was designed to help babies and toddlers not beginning to eat table foods, the steps inside will be instrumental in helping your child begin to eat food too, no matter what their age!
Get the How to Transition to Table Foods Printable
Alisha Grogan is a licensed occupational therapist and founder of Your Kid’s Table. She has over 15 years experience with expertise in sensory processing and feeding development in babies, toddlers, and children. Alisha also has 3 boys of her own at home. Learn more about her here.

I would love to go more in depth, my son who is in ESCE rather than full time, year round home ECI because he is 3 now (Elliott has down syndrome, and was already going to be given one at birth as he was born at 28 weeks, but he had a duty on trees yet as well as some issue that did not connect his esophagus to his stomach. They did not feel comfortable working on that until he was “adjusted to term” lb which was about… 108 days total in NICU, but to 38 weeks… That was a very scary surgery he is now curious and he has come a very long way, but when I’m thinking about the concept of chewing it’s so much overwhelming… He did get for the summer a occupational therapist but unfortunately there was a personal emergency loss, something that we had to be understanding of, that we can’t find a Medicaid/CHIP or oral therapist. I have to agree, the Z vibe tools helped so much! He still screams when we brush his teeth but as I like to joke around, he is in a late state of the terrible twos due to his developmental delays & just doesn’t enjoy any life sustaining activity outside of playing around… So maybe that’s why although he doesn’t react as poorly as he would have, when he was 18m…
My dad spent a lot of time with him and he is pretty sure that he will not be too dependent forever and it might be not an option until he understands what we are saying more, and we can understand him more.
He isn’t nonverbal but he gets very frustrated when he can’t communicate and this is a pretty common thing that children’s with down syndrome deal with I believe.
But, I was wondering if you had any specific advice for children with extreme developmental delays such as or including down syndrome.
Thanks
Hi Sadie,
Thanks for much for this information, and I’m happy to hear that things are improving for your son. No small part due to your diligent work and efforts! While we don’t have any specific articles for kids who have more extreme delays and needs, we have a ton of resources on different topics that may be helpful. Here are some strategies for tooth brushing as well as one on oral aversion which may help! There are many links within those posts that might be beneficial.
Thanks so much
Laura
Your Kid’s Table team member
My daughter was born with a heart defect and went into heart failure around 2 months old. She got an NG feeding tube at 3 1/2 months old because she was losing weight. She is now 13 1/2 months old and her heart is in much better shape after open heart surgery and some time.
But trying to get off the tube … That’s hard! She takes solids now and she will drink water but only tiny amounts of milk. She’s doesn’t know how to take in enough to satisfy her hunger and keep her growing.
And having an active baby or toddler with a feeling tube can be quite challenging. I recently wrote a post with some tips on how to manage a baby with an NG Tube (https://mamarissa.com/life-with-an-ng-tube-baby-my-tips-tricks/) but I’m always eager to hear any other tips and tricks anyone else has!
We have a feeding therapist, GI doctor and nutritionist helping us make decisions about her feeling, along with her cardiologist. A lot of what you mentioned here are things her feeding therapist has worked on or instructed us to do. We are hoping to begin a tube weaning process soon but I’m honestly a little scared of what it might take for her to learn how to feed herself enough.
Do you have any recommendations on the best way to teach an NG tube toddler how to eat enough to sustain her?
Hi Marissa!
This can be very tricky, and it sounds like you have a great plan and a team who can help work toward this goal! It honestly sounds like you’re doing all the right things, my only other suggestion would be to work on her interoception sense so she can start connecting hunger cues to feelings, since this is an issue when kids have been tube fed.
Best,
Laura
Your Kid’s Table team member
Hello,
My son is 28weeks Preterm baby born on 18th May 2023. He is now 1year 4months of age. Since birth he is on nasogastric feeding tube.
Below are the medical details of my baby.
Gender:Male | Birth Weight: 1273gm | Current Weight: 6.450Kg
After birth he had breathing difficulties so was on mechanical ventilator for 7 days. He is a Bilateral Cleft lip and palate.
We and our doctors are trying our best to make baby comfortable swallowing milk/water. However due to open palate he finds it difficult. Few of the doctors suggested that it is risky to push as he might aspirate. Thus we need to wait for his palate closure.
The problem here is that he is not gaining weight on liquid diet and also getting food aversion & sensitive to taste or smell. Sweet, sour, spicy all kind of taste makes him feel like puking.
I understand G-Button is a solution to introduce semi solids but as you can see we already have a lot of operations for kid and dont want to introduce new.
Is there a way to gain weight on NS-Tube so that he reaches atleast 10Kg to 11Kg in 6 months time and we can then plan for palate closure?
Thanks.
Hi Omair,
It sounds like you guys have been working so hard to help your kiddo thrive. In any instance where aspiration is a possibility and concern, we need to be extremely careful with introducing changes. I would expect your feeding care team to be working to evaluate if his current formula is appropriate for his growing needs. Have they raised concerns over his weight? There are certainly ways to increase the caloric intake through an NG tube, but due to the medical complexity, I am unable to make recommendations apart from consulting his full care team. I would be persistent with them that you are concerned he is not growing at the rate you expect for his age. A G-button is certainly an option but as you said, that is another procedure, so personally I’d work with his current care team to address the NG tube first.
Best,
Laura
Your Kid’s Table team member
My son is about 12 months old and currently has a Ng tube for aspiration. He is eating purées but refuses to take milk by bottle or sipy cup. GI doctor wants us to start giving him liquids to honey thick for about a month so we can remove the tube. Any recommendations to help my baby get onto with the oral drinking ?
Hi Zuhair! We strongly recommend working with a feeding team for the weaning process, I know it’s not always possible, but please stay in close communication with your doctor as a minimum. For drinking, you’ll again want to make sure it’s safe to start working on liquids, and if so, which kinds. Milk and formula are thicker than water and therefore easier to manage. Whatever liquid you start with, you’ll want to try putting a little bit on a spoon and seeing how they manage with it. If you’re in feeding therapy, the therapist should try this first. You’d then keep practicing from a spoon and then experiment with a sippy cup or straw cup. But, keep in mind that it requires a lot of oral motor skills and sequenced swallowing to do either. Consistently working on these strategies and being patient with what can be a long process are a very important part of this transition!
Best,
Kalyn
Alisha, your article is SO HELPFUL in understanding my child’s oral aversion, so THANK YOU. Do you have any posted material regarding older kids with this problem? You wrote that a lot of techniques apply to all ages, but most of the information is about young child issues and solutions. My son isalmost 8yoa and has Esophageal Dissecans (unexplained sloughing of esophagus). He ultimately quit eating or drinking at all. It was hurting his stomach but we didn’t know that at the time. He would get really lethargic at times also. Fast forward to our trip to the ER, his diagnosis and treatment. Even after effective meds, he still REFUSES TO EAT OR DRINK, so he’s had an NG tube for 8 days. We’re back home now and He wants it out but it’s so hard for him – he’s scared eating will hurt. Yesterday he ate half of a saltine cracker and said it only hurt his nose from the tube, but he hasn’t eaten since. That’s his first food/oral intake in 12 days. I don’t think he wants to try it again. He drank a bit of water today and said it didn’t hurt – who knows if he’ll do it again. He gets sad and seems depressed at times. He needs to go back to school, but he’ll have the NG tube. We have an appointment with a feeding therapist but it’s 2 weeks away. Any articles or info for his age would be great. (But thanks to your posts, I understand a bit why he’s even refusing to brush his teeth or suck on a sucker, etc.).
I have a 5 yr old who does 12 over night feeds. She never gets good sleep. What can I do instead of a 12 hr feed. She also gets 3 feeds during the day if she doesn’t get enough food, but what is enough for a 5 yr old. Our nutritionist is new and doesn’t seem to help us much. Thank you.
Hi Mayra! Thanks for reaching out! Have you tried discussing this with your pediatrician? Or perhaps speaking to a different nutritionist? It would be helpful to discuss further with your pediatrician, since they would know more about her needs and medical history.
Best,
Kalyn
My granddaughter has had a feeding tube since birth due to a bad heart. A few months back she had started taking small bites of different things and seemed to enjoy it. Then she caught a virus. Since then , no matter what we try she refuses and often gags just at the sight if food on her spoon, even the tiniest amount. She is now almost 14 months.
We have been told that some never learn to eat and i pray this wont be the case. Any advise would be greatly appreciated . Thank you
Hi Loretta! So sorry to hear about your granddaughter’s tough journey so far, but please don’t lose hope! We understand how stressful and frustrating it all can be, but we’re here to help! Oral aversions are common after getting sick. Keep offering without pressure. Some oral motor exercises may help too! Here’s a list of some ones to try!
Best,
Kalyn
Please let me know what’s happening with your granddaughter? My granddaughter had a heart transplant and is 2 years old now. She has a feeding tube in. She is able to eat solid foods fine. It’s the drinking that’s the problem for her. Any information you can pass along would be appreciated.
Hello, I am a new OT grad. I have a case with a child with a G-tube. Do you have more tips for oral play like other oral toys to use and how to use them? as well as what type of foods you use to start and how?
Hi Amberlie! Thanks for reaching out! We have a post with tons of Oral Motor exercises to try! And as for the type of foods to start with, try baby foods, yogurt, or homemade preferred foods. Just make sure the food is totally smooth. It should have no textures at all in the beginning. Hope that helps!
Best,
Kalyn
My son , born at 30 weeks , was taking bottles in combination with NG tubes for feeds while in the NICU. As his feeds got larger and reflux increased, his daily percent of oral intake went down. We began to see GI, nutrition, and an SLP and are still trying to combat overal aversion ( signs of disgust and gagging when we try to introduce a bottle). Since we completely stopped bottles, we feel as though he has forgotten to even suck and instantly uses his tongue to play around with the nipple or pacifier and push it out a bit or roll it around in his mouth instead of latching It sucking it like he once used to. Any recommendations on best way to ween him off NG tube and introduce him back to sucking versus using his tongue to push out? Thanks!
Hi Charlie! Thanks for reaching out! We would definitely recommend working 1:1 with a feeding therapist if possible- consulting with your team of GI, nutrition, and SLP to assist with weaning off the NG tube. In the meantime, a good activity that promotes oral motor skills (which can help with sucking) are to practice making all kinds of silly faces at each other and in the mirror. Kissy faces and noises are really helpful and can also be a fun activity for the two of you! We have more oral motor exercise ideas here! Also, keep practicing with a pacifier a few times a day to help him get used to the feel of the nipple and motion of sucking again. Hope that helps!
Best,
Kalyn
I’m sorry to hear this. How’s it been the last month? This sounds exactly like my daughter, if you have any positive suggestions. Thank you.
Hi Ben! For the last three months since he’s been home with an NG tube we’ve had positive success with combating the oral aversion. He now happily puts everything in his mouth and love gnawing at his teethers and hands. We also do a lot of positive oral stimulation exercises right at the start of his feeds and let’s us even put the bottle nipple and glove finger dipped in milk in his mouth for quite a while! Give it time but positive oral stimulation techniques will help to combat the aversion. Try singing and smiling and laughing with every oral stimulation and try to be consistent! Eventually they’ll learn to associate it with positivity and hopefully overcome that aversion.
Now we are faced with another challenge- it’s as if he’s forgotten how to latch and swallow from the bottle nipple. Instead he plays around with it and gnaws at it instead so we haven’t been successful in being able to get him to take milk from a bottle still. This is our new challenge that we are trying to figure out ourselves for more than the past 1.5 months but haven’t been successful. If you’ve tried anything that works please do share!
Hope this helps- let me know if you have any other questions or any other way I can help. 🙂
Thanks so much for your quick response. Our journeys sound really similar. Our daughter did 101 days in the NICU and came home taking 40% PO and the rest through her NG. After two weeks at home, she was up to almost 70% PO, but has steadily declined over the last two months. Now we are lucky if she takes 10 mls once or twice a day. She also has two large vomits each day during or after feeds. Doctors thought they saw pyloric stenosis on her ultrasound, but it turned out it was not. We’ve tried fortifying with different formulas, removing milk from my wife’s diet, and gelmix with no luck. We just switched our doctors and have a repeat swallow study coming up, so let’s definitely keep each other posted. Thanks for the advice and support! I’m sorry I don’t have much advice in return, but know you are not alone.
We ran through similar tests because of his reflux. We did a swallow study at the NICU, upper GI study to rule out any mechanical issues, and GI motility study to make sure gastroperesis didn’t play a factor – all came out negative which makes us think it’s the normal newborn reflux due to immature esophageal sphincter and it may just be time that will help. I’d recommend getting a gi specialist on board to help and seeing if any of these other studies are beneficial to rule out any other causes. We started our soon on pepcid 0.3 twice daily since our first visit to GI and it has helped tremendously ( we also tried weaning him off for 2 days wondering if it’s still needed and it was confirmed instantly that it is making a huge difference in a positive way so we are keeping him on it until further notice). The spit ups and arching reduced drastically even though there was still some
Vomiting present. I switched to a vegan diet and removed all Dairy and soy from my diet for over a month and each stool test came back negative. To try to resolve the last but of spit ups/ vomiting we just switched over to Neocate Syneo which is a broken down formula which we read was great for reflux and potential allergy babies… we are on day 4 of 100% formula and seeing a lot less spit ups but think he still needs time for transition since he is showing to be uncomfortable for anywhere between 5-20 mins right after the feed is done. If you are looking for a formula for the same reasons I’d recommend this one- we selected it after tons of research trying to decide what would be best for a trial run and moving onto the next steps. Our gi doctor recommend a two week trial so patiently waiting to see where we end up. The sooner the baby is able to sit up and use their core the sooner the reflux will hopefully decrease so we are doing exercises to focus on those core muscles.
Thank you so much for this great advice. I had no idea about the correlation between core strength and reflux, so that gives me extra incentive when we do PT. I’ve also been looking into changing her reflux medicine (currently Prilosec) and am going to ask about switching to Pepcid. I apologize for my late reply as the last few days have been eventful. What originally drew me to your post was the description of your son’s tongue action at the bottle. It sounded just like my daughter, who had been declining from 70% PO when we were first home from the NICU to basically zero. The other day, our Early Interventionist was over and saw this tongue action for the first time. She encouraged me that this was interest, not aversion (which we had been so cautious and concerned about), and to fill the nipple halfway and keep it in my daughter’s mouth. Sure enough, after ten minutes of patience (and stress), my daughter focused what she was doing with her tongue/mouth, latched, and drank 1.5 oz. We were obviously shocked. This was more than she had drank during a feed in over a month. Since then, it’s been a bit of a rollercoaster. She’s been drinking anywhere from 0-50 ml. Sometimes, she’s latched well in under a minute. Other times, it’s taken 20 minutes of waiting (and wrangling) before she latches and drinks. Sometimes, she hasn’t latched at all. She’s still vomiting 1-3 times/day (including throwing up her tube twice the other day), but seeing her drink has given us a desperately needed boost. I know every child is different, but I share this information with the hope that maybe it can help (if indeed our little ones are dealing with the same challenge). Please keep me posted! I truly appreciate your help and support.
Wow, that’s great!! I’m so happy to hear the nipple in the mouth technique worked for you, the little rewards mean everything! … it definitely is a slow process and requires so much patience, reading this was a a good reminder to me that outcomes will come with some patience.
How old is your little one if you don’t mind me asking?
Today we took my son’s tube out (formula was getting clogged at the bottom) so we waited a little longer in an attempt to now increase / reinitiate his hunger drive. It took 6 hours for him since the last feed to show crying/ hunger queues! ( at the same time we were closely monitoring hydration and tracked how much he needed to prevent any issues) . I tell you this because one thing you don’t want your child to lose is the natural ability to get hungry which became inevitable for us as he transitioned to taking 100% tube feeding only. It’ll be a slow process but we were so glad today to see him get hungry naturally 🙂 my recommendation is to hold off on a long bottle break and keep introducing it if there’s no aversion, it’ll prevent diminished or loss of hunger drive in the future and hopefully they’ll retain the techniques needed to latch properly! We were also told by our gi dr that long continuous infusions lessen the natural ability to get hungry so as if today we are revising his daily feeding schedules to remove his continuous overnight feed and spread it throughout the day , fingers crossed!
I’m hoping for the best for you guys, positive vibes only! Sounds like it’s heading in the right direction so continue doing with what you’re doing 🙂
Hi Charlie
I’m Parvathy. My son is 11 months on 19th.He is under ng tube. He’s having an oral aversion because he has cow milk and soy intolerance so he’s vomiting since 3 months before that he was struggling to burp and having tummy pain too. He is hospitalized for two times for his failure to thrive and weight loss. He also have bad acid reflux too. While hospital stay they ruled upper GI X-ray and it looks normal and also did ct scan too everything looks normal. He refusing bottle so they put ng tube. He’s not taking any solids. We tried to feed and wean him about a week without ng tube. He’s not taking much so his weight reduced again. Do you have any suggestions? He is still laying down and rollovers. GI suggested Neocate syneo we’re giving it through ng he’s not taking it by mouth bcz of its bad smell and taste. Please reply back. TIA
Parvathy
How is the baby now I’m going through this now and I’m desperate for information and for my son to start eating
Hi Charlie,
Sorry that I have been off the grid. We waited weeks for our daughter’s repeat swallow study and when the day came she did not drink. Obviously crushing, but we press on and keep trying! We had family come to town that same night, which helped us move past it. Seeing others interact with her always allows me to regain perspective! Our daughter is 5.5 months but 3 months corrected. How about your little one? The SLP at the study recommended only bottling her 3x/day. We understand there are benefits to a PO break, but agree with what you said in your post about not wanting her to forget how to suck and swallow. When she does drink, it’s always one run and then she won’t relatch (one doctor called this “drinking enough to take the edge off”). She also continues to have bottle encounters where she demonstrates strong hunger cues but does not latch at all. I’m curious to hear how your new schedule is going since you’ve eliminated the overnight tube feed. I’d love to allow our little one to sleep for longer stretches!
All the best,
Ben
My daughter is 9.25 months (6.75 corrected) she has had an ng tube since birth. Oral aversions, will not take a bottle or sippy cup and if she does it’s only about 10mls over 20-30 minutes which only comes out because she’s biting it. Will not take pacifier anymore. Started purées and was going well for about a month but recently has been vomiting on occasion during tube feeds and not wanting any purées anymore. She had an upper GI study in the nicu at 4 months and was aspirating every 2-3 swallows. She’s still waiting on a follow up study but hasn’t shown signs of aspirating since then up until recently. She’s on omeparazole and has GERD. She is primarily tube fed, we started weaning her at around 5 months and she did well… then once we were almost there she went 10 steps back and started back to all ng feeds as she drastically lost weight. I’m at a loss of what to do, and my heart breaks for my little girl. She’s followed by her Pediatrician, RD and SLP and we still haven’t had clear guidance or help as to how to move forward.
I try with purées daily and sippy cups and try to keep it positive but lately she has been absolutely refusing everything, is it possible that she’s gotten solids in her lungs and is now associating that discomfort to purées?
My son is not drinking and eating anything from last 6 months.
Currently he is on NG tube.
He born at 26+1 weeks..
Please help me on, how to ween of NG tube.
Hi Lakshmi,
Hugs! We know it can be so challenging to have a little one not eating by mouth. Weaning off an an NG tube is a process that is really specific to each kiddo. So we would definitely suggest talking to your child’s doctor about getting your son set up with a feeding therapist. It is likely that the doctor will also want to run some tests (like a swallow study) to make sure that it is safe for your son to eat by mouth. HERE is a good introduction to feeding therapy. Please reach out if you have any questions at all!
Best,
Andrea
Hi
My son is having milk from the bottle when he discharged from hospital and suddenly stopped drinking. Doctors said it is common for the babies who has reflex symptoms. It’s been 8months since he moved to NG tube. Inbetween I have introduced solids he had purées nicely and no he is refusing purées also. Please help to come out of NG tube.
Thank you,
Lakshmi
My little one is two and half and has has been on the gtube for a little over a year . Due to him having chemo. The chemo and along with the constant medications we have sometimes given him by mouth has caused a strong oral aversion. ALONG with a extreme distrust of people trying to feed him. Only thing he will allow us to give him is water. Please help
Hey Crystal,
That sounds like it’s been a tough road for you guys. If he’s cleared to eat by mouth, giving him as much control as possible might be helpful. You could do a straw or spoon dipped into different flavors to let him try (you modeling yourself) to start with. Working directly with an experienced feeding therapist might be helpful. You could also check out our free table foods school workshop to give you some more ideas! You can save your seat HERE.
Best,
Andrea
Hi lakshmi im going through similar experience, any luck ?
the feeding team helping my special needs son, turned his high chair towards the wall when he refused to cooperate with their techniques i turned the chair back and they left was i wrong?
Hey Helen,
Oh it can be really challenging when you’re not comfortable with what the therapists are doing. I’d suggest setting up a time to chat with the feeding team and to get a better idea of the types of techniques they use in their practice. A behavior approach tends to use a more reward based technique and a child-based based approach tries to follow the child’s lead while addressing underlying sensory and oral motor challenges. Feeding can be a huge challenge for the whole family, so it is helpful if everyone is on the same page for your peace of mind. I’d suggest taking a look at our feeding therapy guide to give you a little more details on what to expect! I hope that helps.
Best,
Andrea
My son is about to be 5 months and trying to help him is so stressful because I can’t work because daycare don’t won’t the responsibility he loves to pull his ng tube out I really hope when his therapist comes she help him seem like he’s really referring the bottle now cries so hard so I just put it through the tube because I don’t won’t him to feel focus someone plz help me relax to help him.
Forced I mean he also didn’t start oral till he was 3 months due to Complication in the hospital and also having surgery.
Hey Briona,
When little ones start pulling out their ng tube, it can be so stressful! Hang in there, you’re not alone! This unfortunately happens a lot. It sounds like he is working closely with a therapist, which is great news. It’s so helpful to work 1:1 with someone while weaning off of any type of tube feedings. His therapist should be able to tell you if he’s ready for a bottle or not yet, each little one is different. Once you get the go ahead, introducing the bottle really slowly is important- just a little milk at time. Try to encourage your little one to be in a calm state before starting. Sometimes pacifiers can help little ones get used to the idea of sucking before introducing an actual bottle.
Best,
Andrea
Hello, my baby was on a ventilator till she was 3 weeks. When she came off the ventilator we tried to give her a bottle but she was aspirating. She Gtube at two months and we were able to take her home. We would practice with her using a preemie nipple and she will do good drinking her milk. But now she just bites the nipple (she’s been doing that for about a Month). Now that she’s 6 months we are trying baby food and she eats it’s with no problem. Can you please tell me how can I help her drink her milk?
Hi karina, going through a similar problem where now it’s as if he’s forgotten how to suck the nipple of the bottle and drink milk. All he does is move it around in his mouth and bite on it but doesn’t drink form it anymore. Now rely solely on NG tube 24/7 to feed him milk. Any suggestions or luck with your little one?
My daughter takes things/spoons/toys in her mouth. She will accept the bottle in mouth but does not suck on it. She has ng tube from birth till now (8 months). She was in hospital for 6 months due to complex medical conditions but is cleared to try oral. Help me with some tips to get her sucking.
Occasionally she accepts purees mixed with her formula
Hi Larissa,
It sounds like you guys have had quite the journey! We’re so happy to hear that your daughter is home from the hospital and that you guys are working on feeding:) We definitely recommend working 1:1 with a feeding therapist if possible. You can learn a little more about what to expect from feeding therapy HERE. A favorite activity that promotes oral motor skills are to practice making all kinds of silly faces at each other and in the mirror. Kissy faces and noises are really helpful and can also be a fun activity for the two of you! You guys aren’t alone in this journey 🙂
Best,
Andrea
Your Kids Table Team
Hi Larissa,
Hope you are doing good!
My son also with the same situation, currently he is on NG tube feeding from last 7 months.
We would like to know how to ween off the NG tube.
Appreciated your help on this..
Thanks,
Lakshmi
Hi Larissa, going through a similar problem where now it’s as if he’s forgotten how to suck the nipple of the bottle and drink milk. All he does is move it around in his mouth and bite on it but doesn’t drink from it anymore. Now rely solely on NG tube 24/7 to feed him milk. Has been in an NG tube for 6 months now , with 3 months solely on tube only no bottle. Any suggestions or luck with your little one?
please forward this article to me.. I am trying to wean my son off tube feedings.
Hi Tasha,
I just sent you the link to the article!
Best,
Andrea
Hi,
Can I please have the article too.
My son is 12 weeks and NG fed, he has hyperinsulisum so needs to have his full amount of milk.
He will take 40mls orally , occasionally more & sometimes
less.
He suffers badly with reflux so this is the main reason for the tube.
Thank you
Hi Jemma! Here’s a link to our blog post about tube weaning. Hope that helps!
Best,
Kalyn
Yes myself as well my baby does try things but can be better