Learn exactly what this new diagnosis of Pediatric Feeding Disorder (PFD) means for picky eater kids, how it differs from ARFID, and how to help kids overcome PFD with ways that align that with positive parenting.
Have you heard the news?
As of October 1st, 2021 there is a brand new diagnosis for kids. It’s called Pediatric Feeding Disorder, or PFD, and is much needed.
As an occupational therapist that specializes in feeding, my hope is that it helps parents understand their child’s feeding challenges better and that it helps professionals give kids the right strategies and treatment.
Why Is There a New Diagnosis?
Honestly, there’s been a lot of lack of clarity in the feeding therapy world about which kids actually have a feeding problem and how to categorize them. In our culture, and even around the world, “picky eating” is a subjective and broad term.
Children that don’t like veggies can be called picky eaters.
Children that prefer kid’s foods like mac and cheese, chicken nuggets, pizza, and hot dogs, but will eat a variety of those foods and still some fruits and veggies are called picky eaters.
Children that eat only 10 foods (or less) and gag (or vomit) when a new food is put down in front of them are called picky eaters.
Do you see the problem?
Clearly, all these kids aren’t the same. This confuses and frustrates parents whose child fits in or around that last example because they have no other way to explain how difficult eating is for their child.
Frustration reaches new depths when basic picky eating tips and strategies are used and there is no progress.
This new diagnosis clearly defines, what I often refer to as an extreme picky eater, and that’s important because now parents and the professionals that help these kids have a language, and now treatment, for kids that have been previously been known as super picky eaters.
And Feeding Matters, an advocacy non-profit, sites a conservative estimate from the Journal of Pediatrics that 1 in 37 kids under the age of 5 are struggling with PFD. That’s a lot of kids, and it’s not even including kids ages 6 through teen years that are also quite capable of having PFD.
The diagnosis is obviously needed.

The Difference Between a Feeding Disorder and an Eating Disorder
In the last 5-6 years, there’s been a lot of confusion in and around the feeding therapy community about the diagnosis Avoidant Restrictive Food Intake Disorder, or ARFID. ARFID was added as a diagnosis 6 years ago. On the surface, ARFID seemed like it may be the diagnosis that would finally fit this group of “extreme picky eating kids.”
But, if you read the details of this diagnosis, there is at least one very important distinction. ARFID is an eating disorder, not a feeding disorder.
Eating disorders are psychiatric diagnoses. Meaning, they’re caused by the way an individual *thinks.* ARFID therefore is in the same category as Anorexia and Bulimia.
A child that has trouble chewing, has undiagnosed reflux or a myriad of other often hidden medical issues that affect appetite and eating, or sensory processing challenges that affect their ability to accept different foods has a feeding disorder – not an eating disorder.
The difference is that a feeding disorder means a child has a problem with the skills needed to eat OR the physical feelings caused be eating. This can, and often does, result in kids from infancy through teens to have strong emotional reactions to new or different foods.
Yes, some behavioral components develop as a result, but it’s all rooted in an underlying cause that hasn’t been addressed. And, so many kids aren’t identified as having an underlying cause. It takes a skilled professional in some cases to discover the underlying cause.
That is not the case with an eating disorder such as ARFID.
What Is Pediatric Feeding Disorder or PFD?
Pediatric Feeding Disorder is a diagnosis given to children that don’t have appropriate nutrition for their age, which may mean a child is still eating pureed foods or only drinking a bottle/nursing past a year old, has minimal or no fruits/vegetables/protein sources in their diet, or eats only soft or crunchy foods.
Children with this diagnosis commonly eat 20 or less foods and struggle to eat new foods because of underlying difficulties with oral motor skills, sensory processing, or medical conditions such as food allergies, reflux, or EoE, to name a few.
These underlying causes may not be known to parents, and children with this diagnosis often struggle with their eating difficulties for 2 or more years, unless the child is diagnosed in infancy or as a toddler, which is possible.
You can complete this questionnaire from Feeding Matters, a non-profit that was instrumental in creating this diagnosis with a team of feeding therapy experts, to find out if your child may have PFD.
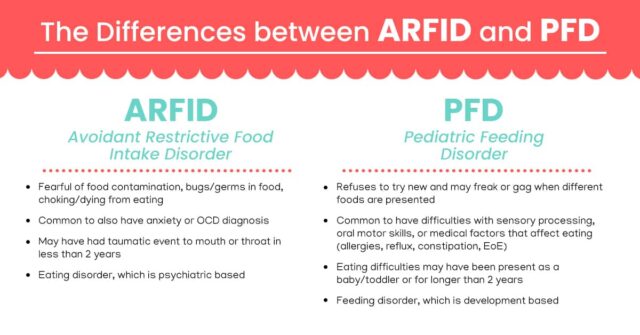
How Is ARFID Different from PFD?
While we already talked about ARFID being an eating disorder and PFD a feeding disorder, there are some other helpful distinctions if you’ve ever wondered if your child has ARFID. Or, if your child has received an ARFID diagnosis before PFD was available.
If that’s the case, you may want to check in with professionals that understand PFD to make sure ARFID is still an appropriate diagnosis.
With both diagnoses, children are often fearful of new foods, but with ARFID, the fear often comes from a place of true psychiatric anxiety, that is often irrational. Kids correctly diagnosed with ARFID will often be fearful of germs on their food, contamination of food, or have a fear that they’ll choke and die.
In some cases, this anxiety is caused by a traumatic event to the mouth or throat. For instance, a child may have a severe choking event that required the Heimlich maneuver, or a medical procedure on their throat.
It’s common for kids with ARFID to have an anxiety disorder or OCD as well.
For kids with PFD, it’s likely they have developmental delays with eating that are related to sensory processing, oral motor, or medical conditions. Here’s a chart to sum up some of these differences.
What Does it Mean if My Child Has Pediatric Feeding Disorder?
Sometimes, hearing that your child has a diagnosis can be scary or overwhelming, but knowing that a child has PFD might be really helpful for you as a parent. Until now, parents with extreme picky eaters haven’t had a way to understand or explain to others what their child was going through.
They’ve had to deal with unwanted and often critical advice from others that doesn’t apply to their child.
Now a parent can say, “My child has Pediatric Feeding Disorder, that’s why they aren’t eating.”
Of course, as a feeding therapist, I’m not suggesting that we close the book there. Quite the opposite, instead, you can begin to help your child now that you know what is going on.
PFD is 100% treatable, I’ve worked with hundreds of kids that have overcome what would now be called PFD.
Kids with PFD do need some specialized help though. If they don’t get it, research estimates that as many as 40-60% won’t outgrow the diagnosis. That means their eating problems will persist.
As teens, this usually affects their social life too.
That’s why it’s critical to address PFD as soon as possible. The younger a child is, the more quickly they’re likely to overcome it. However, teens and even adults are also able to overcome Pediatric Feeding Disorder, even if it’s been many years that they’ve been struggling with eating.
Unfortunately, pediatrician’s have a history of telling parents whose children would now qualify for a PFD diagnosis, to “just wait, they’ll outgrow it.”
Hopefully, now with this clear diagnosis, they’ll be more likely to lead a family to getting the help they need, because a child that is only eating a handful of foods at any age (even if they’re growing adequately) is at a much greater risk of having long term feeding difficulties.

Ways to Help Kids with Pediatric Feeding Disorder
Kids with Pediatric Feeding Disorder will undoubtedly benefit from feeding therapy by an occupational therapist like myself, a speech therapist, or in some cases, a dietician.
It’s important that you seek out a team that specializes in, and is familiar with, PFD. Before you walk through their doors for an evaluation, ask them what types of treatment they use and make sure you’re comfortable with it.
There are two main types of feeding therapy.
The first is behavior and reward based. While you can see some quick wins with this type of feeding therapy, it can induce more trauma and lead to regression.
Basically, a child is asked to take a bite of a new food and they’re rewarded for that bite with a toy, video game, or food they prefer like candy or chips. Or, they may be forced to touch a food, texture, or participate in a therapeutic exercise even though they’re refusing. This may be necessary if a child is critically underweight or has major nutrition deficiencies.
However, as more long term research comes to light, we see that a child directed, skill based treatment gives much better long term results. The only con with this style of treatment is that it initially takes longer to see progress.
However, kids are not traumatized and learn how to eat well with skills that last a lifetime.
I use this second approach, and it’s what I teach in my Mealtime Works program that is designed to give parents a clear daily plan for what they can be doing in their home to overcome extreme picky eating and Pediatric Feeding Disorder.
Many of our students use this program alone when feeding therapy isn’t available and see wonderful life changing results. Some students use it in conjunction with feeding therapy, since the direct therapy is only 1x a week.
Having a home program that parents can follow often accelerates progress and drastically decreases stress in the home.
Other Resources for Kids with PFD
Are Food Jags Affecting Your Picky Eater? What You Need to Know
Pocketing Food Strategies and Causes in Kids
3 Tricks to Get Kids to Eat WITHOUT Their Tablet or TV
Research related to this post:
Bourne, L, Bryant-Waugh, R., Cook, J., & Mandy, W. (2020). Avoidant/restrictive food intake disorder: A systematic scoping review of the current literature. Psychiatry Research, 288, 1-21.
Fisher, M.M. Rosen, D.S., Ornstein, R.M., Mannel, K.A., Katzman, D.D., Rome, E.S., Callahan, T., Malizio, J., Kearney, S., & Walsh, T. (2014). Characteristics of Children and Adolescents with Avoidant/Restrictive Food Intake Disorder: A “new disorder” in DSM-5. Journal of Adolescent
Health, 55, 49-52. doi: 10.1016/j.jadohealth.2013.11.013.
Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Feuling MB, Noel RJ, Gisel E, Kenzer A, Kessler DB, de Camargo OK, Browne J, Phalen JA. Pediatric feeding disorder: consensus definition and conceptual framework. JPGN 2019;68(1):124-129.
Jacobi, C., Schmitz, G., & Agras, W.S. (2008). Is picky eating an eating disorder? International Journal of Eating Disorders. 41(7):626-34. doi: 10.1002/eat.20545
Kovacic K, Rein L, Kommareddy S, Szabo A Bhagavatula P, Goday PS. Pediatric feeding disorders: A nationwide prevalence study. J Peds. DOI: https://doi.org/10.1016/j.jpeds.2020.07.047
Kennedy, G.A., Wick, M.R., & Keel, P.K. (2018). Eating disorders in children: is avoidant-restrictive food intake disorder a feeding disorder or an eating disorder and what are the implications for treatment? F1000 Research. 7: 88. (Version 1). doi: 10.12688/f1000research.13110.1.
Robson, J., Laborda, T., Fitzgerals, S., Anderson, J., Peterson, K., O’Gorman, M., Guthery, S., & BennettMurphy, L. (2019). Avoidant/Restrictive Food Intake Disorder in diet-treated children with eosinophilic esophagitis. Journal of Pediatric Gastroenterology and Nutrition, 69, 57-60.
Walton, K., Kuczynski, L., Haycraft, E., Breen, A., Haines, J. (2017). Time to re-think picky eating?: a relational approach to understanding picky eating. International Journal of Behavioral Nutrition and Physical Activity, 14:62, https://doi.org/10.1186/s12966-017-0520-0.
Alisha Grogan is a licensed occupational therapist and founder of Your Kid’s Table. She has over 17 years experience with expertise in sensory processing and feeding development in babies, toddlers, and children. Alisha also has 3 boys of her own at home. Learn more about her here.
I do think it’s important to note that there is a HUGE overlap in PFD and ARFID! ARFID is a feeding disorder under the DSM-5’s category of Feeding and Eating Disorders. I think the “feeding” part of “Feeding and Eating Disorders” gets missed. An adult with ARFID is often a former child with PFD. As a clinical social worker, I work with both, and both ARFID and PFD can include motor, sensory, psychosocial, and medical concerns. Both really should be addressed via multidisciplinary teams. Just wanted to throw in my two cents.
100% Christina!
Ultimately it comes down to effective treatment strategies, which makes it imperative to know what the underlying cause is. You are so right, there is a lot of overlap, and nuance involved. Fortunately more awareness is growing on PFD in general so that families are able to make informed choices on strategies to help instead of any extreme picky eating behaviors being automatically classified as ARFID and being treated as such- missing a huge sensory component. Thanks for all you do!
Best,
Laura
Your Kid’s Table occupational therapist
Thank you! I would love for all of our fields to actually work together, because adult ARFID clients deserve OT and Speech too, if they need it. And the PFD kiddos deserve clinical social work or mental health counseling, too!
I’m crying right now. I’m almost 16 and I’ve been picky since I was old enough to eat semi solids (literally). I have a very small pallet and can’t try anything new without breaking down. Because of this I avoid eating in public or around people outside of my immediate family who is aware of this. It’s embarrassing to ask for a children’s meal at a restaurant, especially around friends. I want to be normal and be able to eat regularly, but it’s very hard for me. I often end up gagging whenever I’m forced to eat something new, which only further frustrates my parents as they assumed I’m just being dramatic. I’ve spent so long wondering what was wrong with me and avoiding long visits with friends to prevent having to explain that I can’t down a salad. I’m glad this isn’t only me, and I think this could be a step in the right direction to getting better
Sam, I’m so glad you found our blog and that you feel seen and validated. It is NOT too late to improve things. Sensory processing is one of the big underlying causes of picky eating, especially when gagging is involved. Are you following us on Instagram? We share tons of resources there (@yourkidstable). In the meantime, click through the resources within this post, and see if you can start teasing out some of the underlying things responsible for this.
Here for you, ‘
Laura
Your Kid’s Table OT
Hi! My 4 year old son 8/10 times says he’s not hungry when it comes to dinner time and when he does eat all he EVER wants and will eat is Kraft Mac n cheese. We try our best to get him to eat chicken nuggets or fish sticks or some other form of protein but he refuses most of the time or will only take a few forced bites before saying he’s all done. He loves fruit but other than that getting him to eat is a real struggle every single day! Help!
Hi Sarah, have you taken our free picky eating workshop yet? It’s a great starting point for addressing this!
Best,
Laura
Your Kid’s Table team member
We are struggling severely right now with our teen. She had silent reflux and was dx-d with PFD as an infant. At 2 months old, she was taking about 2 oz of milk a day. Failed to thrive. Refluxed out her nose and stopped breathing. She had an apnea monitor and was given an NG tube. No one could help us. Her GI doctor told us to try feeding her sticks of butter. An OT discovered one bottle-nipple that she would actually take. By 15 months, things were looking good.
Here we are over a decade later and she’s doing something similar again. She’s been a “picky eater” and slowly began limiting her diet. This past week, it became severe and she cries because she’s hungry but “can’t eat”. She does struggle with anxiety and sees a therapist. Her anxiety has become worse this past month.
If you are aware of any Houston-area programs or therapists who specialize in this, please let me know!
My 2 year old granddaughter was eating table food really well until approx 2 months ago. She has a very well balance diet consisting of fruit, vegetables, pastas, bread, meat and fish. She now chews her food and spits it out. She is always hungry now. She is trying to say words, but unless one knows what she is trying to say, one wouldn’t understand.
As a newborn she was diagnosed with colic and silent reflux.
My daughter has a doctors appointment in 2 days to get a referral to a paediatrician and a speech therapist.
Any advice you are able to provide would be appreciated.
Regards
Margaret
Hi Margaret! Thanks for reaching out! Since she was eating solid foods well prior to this, it’s a great idea to get it checked out by her pediatrician, who could also refer you to a feeding therapist- if needed. In the meantime, we have a post that talks about spitting out food and offers some tips. Check it out here!
Best,
Kalyn
Can a child have both ARFID and PFD as a diagnosis?
Example: child gags/chokes as an infant/toddler = picky eating due to fear of the foods. Snowball effect + mild ASD = Continues to be a picky eater at age 10 with approximately 10 acceptable foods.
Hey Brenna,
Thanks for reaching out. Technically they can. However if they were previously diagnosed with ARFID, you’d want to make sure that the criteria for PFD is considered now for proper treatment! You can check out more here
Best,
Desiree
I was just wondering the same thing. But you also described our exact scenario so I’m having a moment where I realize we really aren’t alone in this!
can you give picky eater assessment
Hey Tip!
Thanks for reaching out. We don’t offer assessments at this time. The best way to work with us is through one of our programs 🙂 A great place to start is our free picky eating workshop. You can save your seat HERE!
Best,
Andrea