Tongue ties in babies and kids 101! Learn signs of tongue ties and how to treat them if they’re affecting your kids eating, speech, or more.
Frequently in my work as an occupational therapist, I’ve told parents to consider a tongue tie when their child was struggling to eat or take a bottle/breastfeed. Sometimes, what looks like picky eating, is actually the result of a tongue tie, which restricts the tongue from it’s full movement.
The problem is, that while I know what a tongue tie is and the trouble it can cause, it’s not my area of expertise.
Plus, in an online space, you really need an expert’s eyes on your child’s mouth to see if a tongue tie is present and if it’s causing difficulties.
That’s why I’m thrilled to welcome Patricia Pine to Your Kid’s Table to share her tongue-tie expertise as an Orofacial Myologist from Muscles in Harmony. She’s going to share with us the good, the bad, and the ugly of Tongue Ties…
Are Tongue Ties a Passing Fad? A Myth?
Statistically, tongue-tie affects over 5 percent of all newborns. It is three times more common in boys than girls, and there is a genetic link. When a baby has breastfeeding problems, a tongue tie is one of many possible culprits.
When children are toddlers, symptoms may be missed or undiagnosed, thinking that any concerns are part of the growing stages.
Tongue ties are considered Tethered oral tissues (TOTs) and they are very real.
Our son, at two weeks old, had trouble with bottle feeding. He would cry, be gassy/colicky, and drink a bottle so fast I thought the bottle was leaking. He had a dry t-shirt. After his feeding, he threw up the formula time and time again.
What was going on? As an older sibling of nine children, I knew this was not normal, so off to the pediatrician we went four different times.
The pediatrician changed his formula and never looked in his mouth.
Off we went back home to repeat the same abnormal events. Our son was not a happy baby. It was very frustrating of course. At six months of age, he was on the Tommy Tipi cup, so things were much better. As a toddler, he talked up a storm, so speech was not affected.
Not until I was cleaning his teeth (as a dental hygienist) at the age of 20 did he say to me, Mom, this tissue under my tongue gets caught between my bottom teeth!!
I was in shock – what? He stated that he kept forgetting to tell me. I had only cleaned his teeth since he was 18 months old.
I didn’t see his tongue tie, which was a thick, long, webbed frenulum, that’s the tissue that connects the tongue to the base of the mouth. The dentist I worked with at the time released it after the dental cleaning with an ND: YAG laser. Now CO2 lasers are used in tongue tie releases.
I was grateful, but we didn’t know about the therapeutic exercises that assist in preventing reattachment of the tongue muscle. Not until later in my career, during a continuing education course, did I realize why our son could not bottle feed normally.
Our son’s face kept flashing in my head. Clicking, gassiness, reflux, hard tummy, crying, all the symptoms were in front of me the entire time, and I had no idea.
I wasn’t taught this in hygiene school, but after expanding my education, I am well aware of TOTs and how they affect the development and growth of the mouth and physical body.
This information amazes me still today and it’s the reason I wrote the book “Please Release Me – The Tethered Oral Tissue Puzzle (TOTs)”. I had to get the word out!
What is a Tongue-Tie
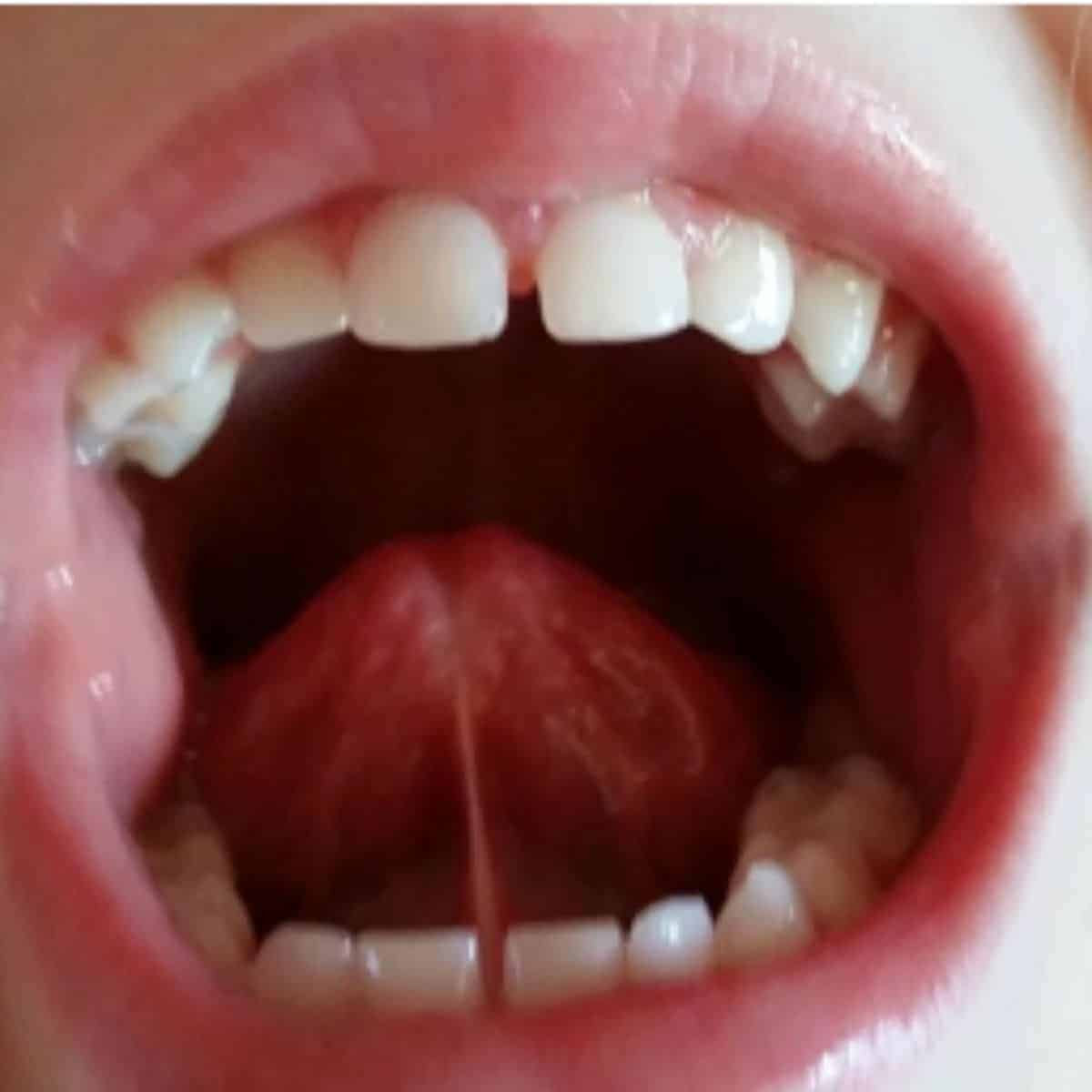
Photo Credit: Muscles in Harmony
The cause of tongue-tie (also known as ankyloglossia) is a simple band of soft tissue called the frenum, or frenulum that has developed as a thick, tight, or short, preventing the tongue from functioning, as it’s job is to shape and mold the upper maxillary arch at the roof of the mouth.
The developmental job of the tongue is to form the upper (maxillary) arch which develops the size of the mouth. If the tongue is anchored or tethered to the floor of the mouth, the tongue cannot provide the size and shape of the upper arch.
How Tongue Ties Affect Breastfeeding
Breastfeeding is next to impossible for the infant to grasp the nipple to express the mother’s milk when the tongue is tethered to the floor of the mouth. Tongue-tie interferes with the ability to latch and suckle at the breast leading to nipple pain, trauma, poor breast milk intake, and more.
Tongue-tie is not the only reason that breastfeeding is a challenge.
A lip tie can prevent the upper lip from flipping upward or flanging to allow the suck, swallowing, and breathing to occur normally during breastfeeding.

Photo Credit: Muscles in Harmony
Buccal ties are included in disrupting breast or bottle feeding; these are found on the sides of the mouth, holding cheeks in place for the ability to speak and swallow. If too tight, the baby or child cannot chew and swallow normally.
Babies need to feed for nutrition and growth, and development. Breastfeeding is a natural bonding method for mother and baby; when this does not occur due to tongue or lip ties, the entire family can be disrupted with emotion and frustration.
Why Does Your Child Need Frenums in the Mouth?
If anyone is wondering why we have frenums. The seven frenums within the mouth are there for a purpose. The frenums hold the cheeks and lips in place to prevent food from falling out of the mouth, create a bolus, and assist in speech sounds.
Have you ever seen a photo of a dog with its head out a car window, and the cheeks are flapping in the fast breeze? They don’t have the frenums humans have.
Our cheeks and lips need to be in place and function correctly. Breastfeeding would not be possible without frenums holding soft tissue in its correct position.
The lingual tongue frenum’s function is to secure the motion of this mobile organ. When the frenum is too tight, thick, or short, restricting the tongue movement and function causes the problem.
Stabilizing the direction of the tongue is vital for speech, eating, and swallowing. Maxillary and mandibular anterior frenums hold the lips in place while talking, eating, and swallowing.
These frenums can cause gum recession (gum shrinks around the tooth, exposing root structure, this exposed root can be sensitive to cold items and decay easily).
During chewing, our tissues are mobile and can pull the tissues away from the tooth when the frenum is too tight or short.
When the upper frenum is too thick and tight it can cause a diastema which is a symptom of a lip tie. These teeth will not come together on their own. If the frenum is released early in life, the permanent teeth may erupt as normal.
How Tongue Ties Affect Other Areas of the Body
Frenums are essential for multiple reasons for a healthy physical body. Frenums can cause the body to compensate for their tightness and shortness and prevent normal movement and function.
Think of “Spiderman”, he throws a spider web around his adversaries to restrict movement. The human body has “fascia” like a spider web to hold the body’s organs and bones in place. It can be fascia induced when a tongue tie creates symptoms such as torticollis.
Torticollis is defined as a consistent head tilt with a limited range of motion.
A sign is a baby who prefers to nurse on only one side, the muscles that connect the collarbone and sternum are shortened (STM), sternocleidomastoid muscle, revealing trouble turning the head which can lead to a flat spot on the baby’s skull.
Tongue-tie, torticollis, headaches, migraines, neck and shoulder pain, swallowing and speech concerns, and behavior issues are only a few of many symptoms created from a tongue-tie. If not corrected, infant torticollis can continue throughout childhood to adulthood.
If these symptoms are not identified, physical concerns can affect the child’s oral growth, development, and behavior.
Signs and Symptoms of Tongue-Tie
Infants
o Difficulty breastfeeding
o Poor seal
o Inability to drain breast/compromised milk supply
o Clicking noise while sucking
o High narrow palate
o Poor weight gain
o Inadequate nutrition
o Gassy/colic/reflux
o Gags easily
o Tongue cupping
o Lateral borders of the tongue lift upward
o Failure to thrive diagnosis
o Difficulty lifting tongue
o Restricted from sticking out tongue
o Heart shape at on the tip of the tongue
o Snoring
o Gets tired breastfeeding falls asleep
o Excessive drooling
Toddler through School Age
o Lack of lip mobility
o The tongue can’t reach the palate
o Frequent gagging
o High narrow palate
o Heart shape tip of the tongue
o Speech concerns, pronunciation of sounds
o Snoring
o Cavities/cavitation on the teeth
o Can’t clean teeth with tongue
o Messy eater
o Difficulty eating (prefers soft foods)
o Frequent ear infections
o Forward head posture
o Tongue posture is low
o Restricts lip licking
o Difficulty Licking ice cream cone
o Abnormal mandible growth
o Delayed tooth eruption
o Hoarding food within cheeks
o Tongue thrush
o Behavior issues
o Allergies
o Add/ADHD
Adolescents to adult
o Poor oral hygiene
o Mouth breathing
o Difficulty licking ice cream cones
o Difficulty French kissing
o Playing a wind instrument
o Snoring
o Loud, messy eater
o Sensitive to hard foods
o Malocclusion
o High narrow palate
o Tongue thrust
o Orthodontic relapse
o Doesn’t like to brush their teeth
o Many more symptoms and concerns
Releasing Tongue Ties
One way to treat tongue ties is to physically release, or cut the tie. The release itself is not pretty, but it is in the best interest of the child or adult having the frenum released.
The lasers available today have many benefits. A CO2 laser is a specific laser that delivers benefits causing minimal to no bleeding, with minimal scar tissue, and is quick and easy in the hands of an experienced professional.
The device used depends on the experience of the person behind the tool. Experience has shown that Diode laser produces more extensive scar tissue, and scissors produce heavy bleeding and scar tissue.
Not all frenums need release; it depends first on the symptoms causing the problems and the length, thickness, degree of movement, and function of all frenums.
The infant, child, or adult can feel tension (i.e., torticollis) within the body as the fascia extends from the tongue to the toes. Tension is not normal, and once a tongue release is accomplished, this may ease that tension and anxiety.
Who Gives Treatment for Tongue Ties… and How??
There is confusion about who should provide the release, what device, and when to have a release completed. The parents or patient should interview this professional, and make a decision based on his/hers knowledge of tongue, lip, and buccal ties.
It’s important to interview the professional because not all professionals know or can recognize tethered oral tissues (TOTS). Some dentists and dental hygienists are aware of ankyloglossia taught in dental and hygiene schools, but aren’t adequately prepared to do a release.
Still, many are unaware of the new methods and classifications, including lip, buccal ties and wound healing.
Medical doctors are not aware of ankyloglossia as TOTs are presented today, many think of tongue-tie as a fad and it’s not taught in medical school.
The doctor chosen to provide the release should have plenty of experience (interview the doctor). They should also recommend 3-4+ weeks (pre-release) of therapeutic exercises to prepare the tissue for release.
If they don’t recommend exercises with a myofunctional therapist, they are not knowledgeable on TOTs and run from that office.
Once the release is complete, post-op therapeutic exercises are necessary for 4-6 weeks for complete success.
The amount of time required depends on the ability of the patient to do the exercises. Preparing the tissue is different for each patient, some need more time for success.
Things have changed in the frenum world. In the last ten years, myofunctional therapy has been brought to the forefront and continues to grow. This professional service has been available for over 70 years and has been underutilized.
A Certified Orofacial Myologist (COM) that provides Myofunctional Therapy is a licensed dental hygienist or speech-language pathologist who received certification from the International Association of Orofacial Myology (IAOM).
These professionals have gone the extra mile in education. Certification requires seeing patients, providing case studies, and being critiqued by an advanced member of the International Association of Orofacial Myology (IAOM).
A comprehensive, exhaustive examination is given to give the therapist a feeling of confidence and knowledge for patient care. It is not an easy exam. This is the only recognized certifying body for becoming a COM.
An infant would depend on the parent or caregiver to provide the exercises, demonstrated by a Certified Orofacial Myologist (COM) that provides Myofunctional Therapy. It’s imperative to finish all exercises for complete success.
The healing process typically takes 3-4 days, letting the body heal itself. After the release of the lingual frenum (under the tongue), observing the opening of the frenum turns into a diamond shape.
This allows for a new frenum to reattach longer with the correct repeated therapeutic exercises. Once released, these soft tissue areas take one full year for complete healing, so ongoing exercises are good.
Many patients or parents feel that once the release is complete, all is good; that is not necessarily true.
Many patients post-release require complete myofunctional therapy to eliminate some of the disorders that the tongue-tie may have caused: mouth breathing, tongue thrusts, forward head posture, snoring, normal breathing, and speech concerns.
A certified myofunctional therapist does an assessment head to toe. Why are there patients who have had orthodontic treatment as a teenager and now their teeth are moving?
This is typically due to orthodontic relapse caused by an unidentified tongue thrust. An Orofacial Myologist can correct or eliminate the disorders based on the cause.
You can think of an Orofacial Myologist that provides Myofunctional therapy as a quarterback. They assess and provide the parent or patient with all the findings at a consultation to determine where to start. You can find a Certified Orofacial Myologist (COM) through IAOM at IAOM.com.
Licensed Dentists, Dental Hygienists, and Speech-language pathologists are currently the only recognized licensed professionals qualified for providing Orofacial Myology.
All tongue-ties are different, and each child or patient is different. This is a non-invasive, holistic treatment. Patients are grateful post-release, releasing the tension in the body. Should you need more information or questions. Contact Pat at her email below.
Want a printable list of symptoms? Check it out at the bottom of the post here.
Pat Pine, RDH, COM™ is a national and international speaker. Pat is a Certified Orofacial Myologist and owner of Muscles in Harmony in Arizona. Pat sees patients virtual or in-person.
Pat is the author of “Please Release Me – The Tethered Oral Tissue (TOTS) Puzzle, which can be found at www.musclesinharmony.com Pat’s’s blog is at musclesinharmony.com/blog/
My 4 year old boy is struggling to speak and pronounce words.his tongue looks like big and it takes all the space in the mouth if he tries to talk
Hi there,
A speech and language evaluation could really help! You can request one from your pediatrician if speech is the big concern.
Best,
Laura
Your Kid’s Table OT
Great info! Thanks for sharing.
Hi Julia! Thanks for reaching out and sharing your feedback! So glad you found this post helpful!
Best,
Kalyn
Excellent Information. thanks
Hi there! Thanks so much for your feedback! So glad you found this post helpful 🙂
Best,
Kalyn
Wow!! Very good information that I plan to share with our team! Thank you!
Hi! So glad to hear you enjoyed this post and plan to share it! Thank you for sharing your feedback with us 🙂
Best,
Kalyn
Yes this sounds like my two year old. He still refuses most table foods and is comfortable with his purées yet he’ll eat fruit and crunchy table foods. He still gags when trying new foods. We r currently working with a certified orofacial myologist. I’m just wondering in your opinion, after the tongue tie lasering when do they typically start eating more foods ? Or will the food aversion be hard to break?
Hi Kristen! Thanks for reaching out! All tongue-ties are different, and each child or patient is different. Generally speaking, once released, these soft tissue areas take one full year for complete healing, so ongoing exercises are good. In terms of the eating difficulties, that can vary as well. Oral motor exercises can also help- especially with the gagging. Be persistent, keep trying/offering, but also being sure not to pressure him. If you need additional help, check out our blog post!
Best,
Kalyn
Hi. My two year old daughter has both a tongue tie and a lip tie which drs refused to cut. She’s now snoring, sleeping with her mouth open, has speech delay and has a high narrow palate. Would getting her tie cut now help her at all?
Hi Nadya, this is definitely at the discretion of an ENT or pediatrician but definitely consider getting a second or multiple opinions if you feel like your child’s needs aren’t being addressed. It sounds like she definitely has some red flags for needing some type of intervention whether that be tonsils, tie cutting, etc. We wish you the best, definitely trust your gut when it comes to this!
Laura
Your Kid’s Table team member